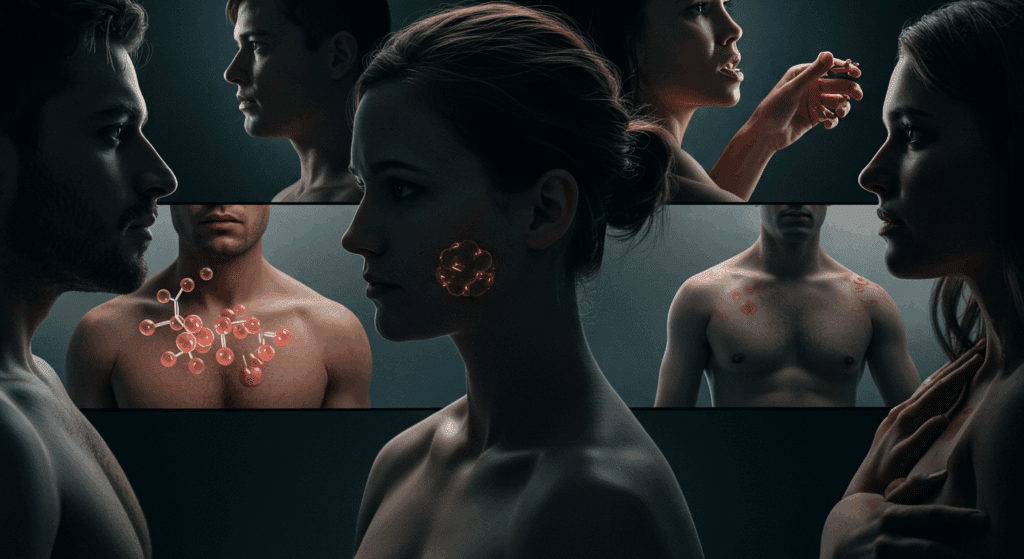
Hormones play a crucial role in regulating nearly every aspect of our health, from metabolism and mood to reproduction and aging. However, the significant hormonal differences between men and women often lead to distinct health challenges and needs. Understanding these variations is essential for optimizing wellbeing, preventing disease, and tailoring personalized healthcare strategies.
Throughout this article, we will explore how hormones influence physical health, mental wellbeing, and lifespan changes, while providing actionable tips for maintaining balance. Whether you’re navigating puberty, fertility concerns, or age-related hormonal shifts, recognizing these patterns empowers you to make informed decisions. By combining scientific research with practical lifestyle adjustments, we can bridge the gap in gender-specific healthcare and promote long-term vitality. For a deeper dive into hormonal health basics, visit The Endocrine Society’s patient resources.
Understanding Hormonal Differences Between Men and Women
Hormones and Their Primary Functions
Hormones act as chemical messengers in the body, regulating essential functions such as growth, metabolism, mood, and reproduction. While both men and women produce similar hormones, their levels and effects vary significantly. For instance, estrogen and progesterone dominate in women, influencing menstrual cycles, pregnancy, and bone health. In contrast, testosterone plays a crucial role in men, affecting muscle mass, fat distribution, and libido.
Additionally, hormones like cortisol (stress response), insulin (blood sugar regulation), and thyroid hormones (metabolism control) function differently based on sex. These variations explain why men and women may experience diseases, medications, and aging processes differently. Understanding these differences is key to personalized healthcare. For more insights, visit The Endocrine Society’s guide on hormones.
Key Hormonal Variations: Estrogen vs. Testosterone
Estrogen and testosterone are often considered the primary sex hormones, yet their roles extend beyond reproduction. Estrogen supports cardiovascular health, cognitive function, and skin elasticity in women, while testosterone in men enhances muscle strength, red blood cell production, and aggression regulation.
Interestingly, both sexes produce small amounts of the opposite hormone—women have testosterone, and men have estrogen—but imbalances can lead to health issues. For example, low testosterone in men may cause fatigue and depression, while high estrogen in men can increase breast tissue growth. Conversely, polycystic ovary syndrome (PCOS) in women often involves elevated testosterone. These differences highlight why gender-specific medical approaches are essential. Learn more about hormonal balance from Harvard Medical School’s health blog.
How Hormones Influence Overall Health
Hormonal balance is critical for long-term health, affecting everything from energy levels to disease risk. For instance, estrogen protects women from heart disease before menopause, while men face higher cardiovascular risks earlier in life due to testosterone’s effects on cholesterol.
Moreover, hormones interact with the immune system, making women more prone to autoimmune diseases like lupus, whereas men may experience worse outcomes from infections. Mental health is also hormone-dependent—women are more susceptible to anxiety and depression due to estrogen fluctuations, while men’s mental health is closely tied to testosterone levels. Recognizing these patterns helps in early intervention and better treatment plans. For further reading, explore Mayo Clinic’s hormone health resources.
By understanding these hormonal differences, we can improve health strategies tailored to individual needs, ensuring better outcomes for everyone.
Hormonal Effects on Physical Health
Metabolism and Weight Management Differences
Hormonal differences between men and women significantly influence metabolism and weight distribution. Testosterone promotes lean muscle mass in men, which increases their basal metabolic rate (BMR), making it easier to burn calories. On the other hand, estrogen encourages fat storage, particularly around the hips and thighs in women, as an evolutionary adaptation for reproductive health.
Additionally, insulin sensitivity varies by sex—women tend to be more insulin-resistant during certain menstrual phases, which can lead to increased cravings and weight fluctuations. Thyroid hormones also play a role, with women being more prone to hypothyroidism, slowing metabolism. Understanding these differences helps tailor diet and exercise plans for optimal weight management. For deeper insights, visit Cleveland Clinic’s guide on hormones and metabolism.
Heart Health: Risks and Protections
Cardiovascular health is strongly linked to hormonal balance, with estrogen providing women a protective effect before menopause. Estrogen helps maintain flexible blood vessels and healthy cholesterol levels, reducing heart disease risk. However, after menopause, declining estrogen levels lead to a sharp increase in cardiovascular issues.
In contrast, men face higher heart disease risks earlier in life due to testosterone’s influence on blood pressure and LDL cholesterol. Furthermore, stress hormones like cortisol affect both sexes differently—women may experience more stress-related heart palpitations, while men are more prone to hypertension. Recognizing these patterns allows for early prevention strategies. For expert advice, check American Heart Association’s research on gender and heart health.
Bone Density and Muscle Mass Variations
Hormones play a crucial role in bone and muscle maintenance, with testosterone boosting muscle growth and bone density in men. Women, however, rely heavily on estrogen for bone strength, making them more susceptible to osteoporosis after menopause when estrogen levels drop.
Additionally, growth hormone and IGF-1 (insulin-like growth factor) function differently between sexes, affecting recovery and physical performance. Men generally build muscle faster, while women may experience greater joint flexibility due to estrogen’s effects on collagen. To support bone and muscle health at any age, proper nutrition and strength training are essential. For more details, explore National Osteoporosis Foundation’s resources.
By understanding these hormonal impacts, individuals can adopt personalized health strategies for long-term well-being.
Hormonal Impact on Mental and Emotional Well-being
Mood Regulation and Hormonal Fluctuations
The connection between hormones and mood is undeniable, with estrogen and progesterone playing key roles in emotional stability for women. During menstrual cycles, pregnancy, and menopause, fluctuating hormone levels can trigger mood swings, irritability, and even depressive symptoms. This occurs because estrogen influences serotonin, a neurotransmitter linked to happiness and well-being.
Men also experience hormonal mood influences, primarily through testosterone. Low testosterone levels may contribute to fatigue, depression, and reduced motivation. However, while women face cyclical hormonal shifts, men’s testosterone declines gradually with age. Understanding these patterns helps in developing coping strategies, such as mindfulness and hormone-balancing diets. For more on managing mood-related hormonal changes, visit Mind’s guide to mental health and hormones.
Stress Response: Cortisol and Gender Differences
Cortisol, the primary stress hormone, affects men and women differently due to hormonal interactions. Women often produce higher cortisol levels in response to stress, partly due to estrogen’s amplifying effect. This can lead to a heightened emotional response and a greater risk of anxiety disorders.
Conversely, men typically exhibit a “fight-or-flight” reaction, with testosterone potentially buffering some stress effects. However, chronic stress in men may suppress testosterone, creating a cycle of fatigue and irritability. Recognizing these differences can guide stress-management techniques—women may benefit more from social support and relaxation practices, while men might prioritize physical activity. For expert-backed stress management tips, explore American Psychological Association’s resources.
Cognitive Function and Hormonal Balance
Hormones significantly influence brain function, including memory, focus, and decision-making. Estrogen enhances verbal memory and cognitive flexibility in women, which is why some experience “brain fog” during menopause when estrogen drops. Testosterone, meanwhile, supports spatial reasoning and assertiveness in men.
Additionally, thyroid imbalances can mimic dementia-like symptoms in both sexes, while cortisol overload impairs concentration. Maintaining hormonal equilibrium through sleep, nutrition, and stress reduction is crucial for mental sharpness. For further reading on hormones and brain health, check Harvard Health’s cognitive function research.
By acknowledging these hormonal influences, individuals can better navigate emotional and cognitive challenges for improved mental well-being.
Hormonal Changes Across Lifespans
Puberty: Different Paths for Boys and Girls
The hormonal journey begins in earnest during puberty, when boys and girls experience distinct developmental changes. In girls, rising estrogen levels trigger breast development, menstrual cycles, and hip widening, typically between ages 8-13. Boys, influenced by testosterone surges (usually ages 9-14), develop deeper voices, facial hair, and increased muscle mass.
These changes don’t just affect physical appearance – they also impact emotional regulation and social development. Girls often become more sensitive to emotional cues, while boys may display more risk-taking behaviors. Understanding these puberty-related shifts helps parents and educators provide better support during this transitional phase. For comprehensive puberty guides, visit KidsHealth’s puberty resources.
Reproductive Years and Fertility Challenges
During reproductive years (typically late teens to late 40s), hormones create monthly cycles in women and daily rhythms in men. Women’s fertility depends on carefully balanced estrogen and progesterone levels, with conditions like PCOS or endometriosis causing imbalances. Men’s fertility relies on consistent testosterone production and sperm health, which can be affected by stress, obesity, or environmental toxins.
Interestingly, male hormones follow a 24-hour cycle (peaking in morning), while women experience monthly fluctuations. These differences explain why fertility treatments must be gender-specific, and why workplace policies should accommodate hormonal realities. For fertility preservation information, explore Resolve’s fertility resources.
Menopause and Andropause: Aging and Hormonal Shifts
As women approach menopause (typically 45-55), estrogen production declines dramatically, causing hot flashes, bone density loss, and metabolic changes. Men experience more gradual testosterone decrease (andropause), with symptoms like reduced energy, muscle loss, and mood changes appearing over decades.
These transitions affect more than physical health – they influence relationships, career satisfaction, and mental wellbeing. While hormone replacement therapy can help, lifestyle adjustments like strength training and stress management often provide significant relief. Recognizing these changes as natural life phases helps individuals adapt with greater ease. For evidence-based aging strategies, visit National Institute on Aging’s health tips.
Understanding these lifespan hormonal changes empowers individuals to make informed health decisions at every life stage.
Managing Hormonal Health for a Balanced Life
Nutrition and Lifestyle Choices for Hormonal Balance
What we eat directly impacts our hormonal health, with certain nutrients playing pivotal roles in maintaining equilibrium. For women, foods rich in omega-3s (like salmon and flaxseeds) help regulate estrogen levels, while men benefit from zinc-packed foods (such as oysters and pumpkin seeds) to support testosterone production. Cruciferous vegetables like broccoli aid in detoxifying excess hormones for both genders.
Beyond diet, lifestyle factors like consistent sleep patterns and stress reduction techniques significantly influence hormonal balance. Chronic sleep deprivation disrupts cortisol and growth hormone regulation, while chronic stress elevates cortisol, potentially leading to insulin resistance. Implementing mindful practices like meditation and maintaining a regular sleep schedule can create a strong foundation for hormonal health. For personalized dietary recommendations, explore NutritionFacts.org’s research-backed guides.
Medical Interventions and Hormone Therapy
When lifestyle adjustments aren’t enough, medical interventions can provide necessary support. Bioidentical hormone replacement therapy (BHRT) has gained popularity for managing menopausal symptoms and andropause, offering a more natural alternative to traditional treatments. However, it’s crucial to consult with an endocrinologist to assess individual needs and risks, as hormone therapies affect everyone differently.
For those with conditions like PCOS or hypothyroidism, targeted medications combined with lifestyle changes often yield the best results. Regular blood tests to monitor hormone levels ensure treatments remain effective and adjusted as needed. It’s worth noting that hormone health is highly individual – what works for one person may not work for another. For current medical guidelines, refer to The Endocrine Society’s clinical resources.
The Role of Exercise in Regulating Hormones
Physical activity serves as a powerful hormonal regulator, but the type and intensity matter greatly. Women often benefit from a mix of strength training and moderate cardio to balance estrogen and cortisol levels, while men may see better testosterone support from resistance training and high-intensity interval workouts.
Interestingly, over-exercising can backfire, particularly for women, potentially leading to hypothalamic amenorrhea (loss of menstrual cycles). Conversely, regular, balanced exercise helps improve insulin sensitivity, boosts endorphins, and promotes better sleep – all crucial for hormonal harmony. Yoga and pilates can be particularly effective for stress reduction and hormonal balance. For science-backed exercise recommendations, visit ACSM’s fitness guidelines.
By combining smart nutrition, appropriate medical support when needed, and balanced physical activity, individuals can create sustainable strategies for lifelong hormonal health. Remember, small consistent changes often yield the most significant long-term benefits for hormonal wellbeing.
Embracing Hormonal Diversity for Better Health
In conclusion, hormonal differences between men and women significantly impact health outcomes, but awareness and proactive management can lead to improved quality of life. From nutrition and exercise to medical interventions, small, consistent changes can help maintain hormonal equilibrium at every life stage. Rather than viewing these differences as obstacles, we should recognize them as unique biological factors that require tailored approaches.
By prioritizing hormone-friendly lifestyles and seeking professional guidance when needed, individuals can mitigate health risks and enhance overall wellbeing. Remember, hormonal balance is not static—it evolves with age, stress levels, and environmental factors. Staying informed and adaptable is key to long-term health success. For ongoing updates on hormonal health research, explore Harvard Health’s hormone wellness guides. Ultimately, embracing these differences allows us to build more inclusive, effective healthcare strategies for everyone.
Image credits Google Labs