The rapid rise of e-cigarettes has sparked intense debate among health professionals, policymakers, and the general public. While initially marketed as a safer alternative to traditional smoking, mounting evidence suggests that vaping carries significant health risks—particularly for young users. From nicotine addiction to potential lung damage, the impacts of e-cigarettes are still being uncovered, making it crucial to separate fact from fiction.
This comprehensive guide explores the latest research on how vaping affects short-term and long-term health, with insights from leading organizations like the World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC). We’ll examine why e-cigarettes have become so popular, their physiological effects, and the ongoing concerns about youth vaping trends. Additionally, we’ll discuss harm reduction strategies and effective ways to quit vaping for those seeking to break free from nicotine dependence.
As regulations evolve and new studies emerge, staying informed is key to making educated decisions about e-cigarette use. Whether you’re a concerned parent, a current vaper, or simply curious about the risks, this article provides a balanced, evidence-based perspective on one of today’s most pressing public health issues.
Understanding E-Cigarettes and Their Popularity
What Are E-Cigarettes and How Do They Work?
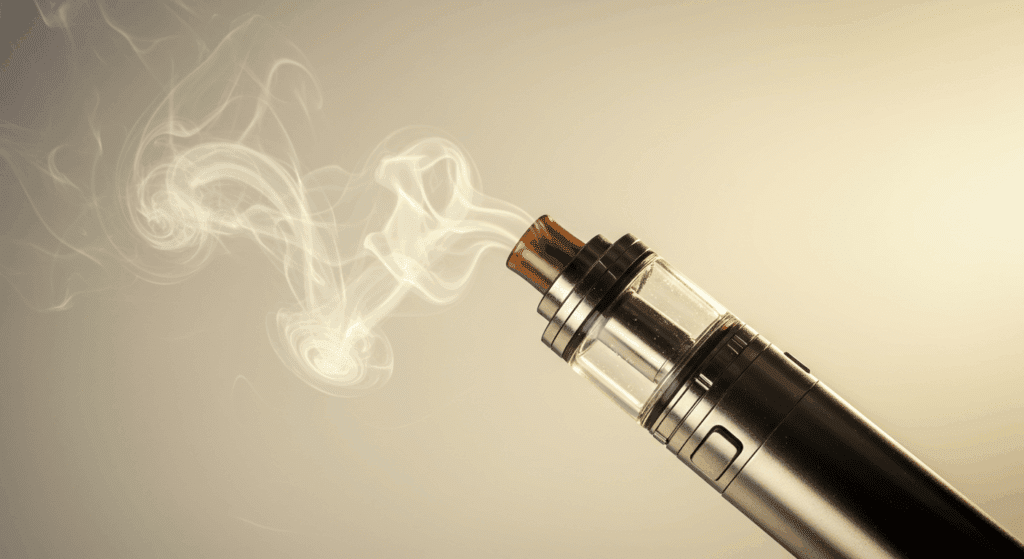
E-cigarettes, also known as vapes or electronic nicotine delivery systems (ENDS), are battery-powered devices designed to simulate smoking without burning tobacco. Instead, they heat a liquid (e-liquid or vape juice) containing nicotine, flavorings, and other chemicals, turning it into an inhalable aerosol. Unlike traditional cigarettes, e-cigarettes do not produce tar or carbon monoxide, but they still deliver nicotine, which is highly addictive.
The basic components of an e-cigarette include a battery, a heating coil, and a cartridge or tank for the e-liquid. When a user inhales, the battery activates the coil, vaporizing the liquid. Some devices allow adjustable settings, increasing or decreasing nicotine intake. While manufacturers market them as safer alternatives to smoking, health experts warn that the long-term effects remain unclear. For more details on how e-cigarettes function, the FDA’s overview provides valuable insights.
Reasons Behind the Rise in Vaping Culture
The popularity of e-cigarettes has surged in recent years, particularly among younger demographics. One key factor is the perception that vaping is less harmful than smoking traditional cigarettes. Additionally, the variety of flavors—from fruity to dessert-inspired—makes them appealing, especially to teens and young adults. Aggressive marketing strategies, including social media promotions and influencer endorsements, have further fueled their growth.
Another reason is the convenience and discretion they offer. Unlike cigarettes, e-cigarettes produce less odor and can be used in more places without immediate detection. However, this accessibility has led to concerns about increased nicotine addiction, even among non-smokers. For a deeper look at vaping trends, the CDC’s reports highlight significant shifts in usage patterns.
Comparing E-Cigarettes to Traditional Tobacco Products
While e-cigarettes eliminate some harmful combustion byproducts found in traditional cigarettes, they are not risk-free. Research suggests that vaping may expose users to fewer toxicants than smoking, but it still introduces nicotine, heavy metals, and ultrafine particles into the lungs. Some studies indicate that dual use (vaping and smoking) is common, reducing potential harm reduction benefits.
Public health opinions remain divided. Some experts argue that e-cigarettes can help smokers quit, while others warn they may act as a gateway to nicotine addiction, especially for youth. Organizations like the World Health Organization (WHO) emphasize the need for stricter regulations to balance harm reduction and prevention. Ultimately, more research is needed to fully understand their comparative risks.
By examining these aspects, we gain a clearer picture of why e-cigarettes have become so widespread—and why their health impacts demand closer attention.
Short-Term Health Effects of E-Cigarettes
Immediate Respiratory and Cardiovascular Impacts
E-cigarettes may seem less harmful than traditional cigarettes, but they still pose immediate risks to respiratory and cardiovascular health. When users inhale the aerosol, they expose their lungs to fine particles, flavoring chemicals, and nicotine, which can irritate airways and cause coughing, throat irritation, and shortness of breath. Some studies suggest that even brief exposure can reduce lung function and increase airway resistance, particularly in those with pre-existing conditions like asthma.
Additionally, nicotine stimulates the release of adrenaline, leading to a temporary spike in heart rate and blood pressure. This cardiovascular stress can be dangerous for individuals with heart conditions, potentially increasing the risk of palpitations or hypertension. Research from the American Heart Association indicates that vaping may harm blood vessel function within minutes of use. While these effects are often short-lived, frequent vaping can compound these risks over time.
Nicotine Addiction and Its Early Consequences
Nicotine is a highly addictive substance, and e-cigarettes deliver it efficiently to the brain, reinforcing dependence. Many users, especially young people, underestimate how quickly addiction can develop. Early signs include cravings, irritability when not vaping, and increased tolerance—requiring more nicotine to achieve the same effect. This dependency can lead to prolonged use and make quitting difficult.
Furthermore, nicotine exposure during adolescence can disrupt brain development, affecting attention, learning, and impulse control. The National Institute on Drug Abuse warns that early nicotine use may prime the brain for addiction to other substances. Even those who switch from smoking to vaping may find themselves maintaining or increasing nicotine intake, rather than reducing it as intended.
Common Side Effects Reported by New Users
First-time vapers often report side effects such as dry mouth, dizziness, headaches, and nausea. These symptoms are typically linked to nicotine intake or the body’s reaction to inhaling unfamiliar chemicals. Some users also experience allergic reactions to specific e-liquid ingredients, such as propylene glycol or flavoring agents.
While these side effects may diminish with continued use, they highlight the body’s immediate response to vaping. Reports from the Centers for Disease Control and Prevention (CDC) suggest that even short-term vaping can lead to unexpected health issues, emphasizing the need for caution. Understanding these early warning signs can help users make informed decisions about their vaping habits before long-term consequences arise.
By recognizing these short-term effects, individuals can better assess the risks of e-cigarette use and take proactive steps to protect their health.
Long-Term Health Risks of Vaping
Potential Links to Chronic Lung Diseases
Growing evidence suggests that prolonged e-cigarette use may contribute to serious lung conditions, including bronchiolitis obliterans (commonly called “popcorn lung”) and chronic obstructive pulmonary disease (COPD). The inhalation of diacetyl, a chemical found in many flavored e-liquids, has been associated with irreversible airway damage. Additionally, the ultrafine particles in vape aerosol can deposit deep in lung tissue, triggering inflammation and potentially leading to fibrosis over time.
A landmark 2019 study published by the American Journal of Preventive Medicine found that regular vapers had a significantly higher risk of developing chronic respiratory diseases compared to non-users. While more long-term studies are needed, current findings emphasize that vaping is not harmless and may pose lasting threats to lung health.
Cardiovascular Risks Over Extended Use
Nicotine’s impact on the cardiovascular system becomes more concerning with long-term exposure. Chronic vaping may lead to sustained increases in blood pressure and arterial stiffness, both of which are risk factors for heart disease and stroke. Research from the Journal of the American College of Cardiology indicates that daily e-cigarette use is associated with endothelial dysfunction—a precursor to atherosclerosis.
Furthermore, the oxidative stress caused by repeated inhalation of vaporized chemicals may accelerate vascular aging. Unlike the immediate spike in heart rate after vaping, these effects develop gradually, making them harder to detect until serious damage occurs. Former smokers who switch to vaping often assume they have eliminated cardiovascular risks, but emerging data suggest that nicotine itself—regardless of the delivery method—remains a major concern.
The Unknowns: Gaps in Long-Term Research
Despite increasing evidence of harm, many long-term effects of vaping remain unclear due to the relatively recent rise in popularity of e-cigarettes. Scientists are still investigating potential connections to cancer, given that some e-liquids contain formaldehyde and other carcinogens when heated. Additionally, the impact of chronic exposure to flavoring chemicals is not yet fully understood.
Public health agencies like the World Health Organization caution against assuming e-cigarettes are safe simply because they haven’t been in use long enough to reveal all consequences. The lack of long-term studies means that today’s vapers are effectively participating in an uncontrolled public health experiment. Until more definitive research emerges, precaution remains the wisest approach for those concerned about lasting health effects.
By examining these potential long-term risks, it becomes clear that vaping carries significant uncertainties—and what we don’t know may ultimately prove just as concerning as what we do.
E-Cigarettes and Youth Health Concerns
Why Teens Are Drawn to Vaping and Its Dangers
The alarming rise in teenage vaping stems from multiple factors, including targeted marketing, appealing flavors, and the misconception that e-cigarettes are harmless. Social media platforms have amplified this trend, with influencers often portraying vaping as a trendy, risk-free habit. Additionally, the discreet design of many devices makes them easy to conceal from parents and teachers.
However, these attractions mask serious dangers. The U.S. Surgeon General’s Report warns that nicotine exposure during adolescence can rewire the developing brain, increasing susceptibility to addiction. Furthermore, studies link youth vaping to higher likelihoods of transitioning to traditional cigarettes—a phenomenon known as the “gateway effect.” Schools and parents face an uphill battle against an industry that spends billions annually to attract young users.
Effects of Nicotine on Adolescent Brain Development
Adolescent brains are particularly vulnerable to nicotine’s effects because critical neural connections are still forming. Regular exposure can impair cognitive functions, including memory, attention, and decision-making. Research from the National Institutes of Health (NIH) shows that nicotine alters dopamine pathways, potentially increasing risks for mood disorders and impulsivity later in life.
What makes this especially concerning is that many teens underestimate their nicotine intake. Popular devices like JUUL deliver nicotine concentrations comparable to a pack of cigarettes, yet their smooth vapor masks the harshness that traditionally deterred young smokers. As a result, adolescents may develop dependence before realizing the consequences, making early education about these risks crucial.
Strategies to Prevent Youth E-Cigarette Use
Combating the youth vaping epidemic requires a multi-faceted approach. Schools can implement evidence-based prevention programs that teach students about vaping’s health risks rather than relying solely on scare tactics. Parents play a key role by having open, non-judgmental conversations and setting clear expectations about substance use.
Policy changes are equally important. The FDA’s enforcement actions against flavored e-cigarettes aim to reduce youth appeal, while some states have raised the purchasing age to 21. However, loopholes remain, particularly with disposable vapes. Community efforts—such as peer-led campaigns and stricter retail compliance checks—can further reduce access. By combining education, regulation, and support, we can help steer younger generations toward healthier choices.
Understanding these youth-specific risks and prevention strategies is essential, as today’s vaping trends could shape public health outcomes for decades to come.
Harm Reduction and Quitting E-Cigarettes
Are E-Cigarettes a Safer Alternative or a Gateway?
The debate over whether e-cigarettes serve as harm reduction tools or gateways to nicotine addiction remains contentious. While some public health agencies acknowledge that vaping may present fewer risks than combustible cigarettes for adult smokers, emerging evidence suggests they may introduce new users—particularly youth—to nicotine dependence. The Royal College of Physicians notes potential benefits for smoking cessation, but emphasizes strict regulation to prevent nonsmoker uptake.
Critically, dual use (vaping while continuing to smoke) remains prevalent, negating potential health benefits. Furthermore, longitudinal studies cited by the American Lung Association indicate many vapers eventually transition to traditional tobacco. This paradox underscores the need for clearer guidelines distinguishing between vaping as a cessation aid versus a recreational product with its own addictive risks.
Effective Methods to Quit Vaping
For those seeking to quit vaping, evidence-based strategies can significantly improve success rates. Behavioral approaches, such as identifying triggers and developing coping mechanisms, form the foundation of many cessation programs. The Truth Initiative offers specialized resources for young adults, including text-based support systems proven to double quit rates.
Nicotine replacement therapies (NRTs) like patches or gum remain FDA-approved options, though some users may require prescription medications for stronger addictions. Emerging digital tools, including quit-vaping apps that track progress and provide motivational support, show particular promise for tech-savvy generations. Regardless of method, setting a quit date and enlisting social support dramatically increases the likelihood of long-term success.
Support Systems and Resources for Users
Overcoming nicotine addiction often requires more than willpower—it demands accessible support systems. Many healthcare providers now incorporate vaping cessation into tobacco treatment programs, offering personalized plans through services like the Smokefree.gov initiative. Peer support groups, both online and in-person, provide communal encouragement and shared strategies for resisting cravings.
Workplaces and educational institutions are increasingly recognizing their role by implementing vape-free policies and offering cessation benefits. Insurance providers are beginning to cover vaping cessation treatments similarly to traditional smoking therapies. By normalizing help-seeking behavior and removing barriers to treatment, we can create environments where quitting becomes not just possible, but probable.
This comprehensive approach to cessation acknowledges vaping addiction’s complexity while providing multiple pathways to recovery—ultimately empowering users to regain control of their health.
Balancing Awareness and Action on E-Cigarette Health Impacts
The discussion around e-cigarettes is far from simple. While they may offer some harm reduction potential for adult smokers, their risks—especially for young people and non-smokers—cannot be ignored. Research from institutions like the American Heart Association and the National Institute on Drug Abuse (NIDA) highlights the urgent need for greater public education and stricter regulations to curb underage use.
Moving forward, a multi-faceted approach is essential. Policymakers must enforce stricter marketing and sales regulations, healthcare providers should offer better cessation support, and individuals must stay informed about the latest findings. For those looking to quit vaping, resources like Smokefree.gov and community support programs can make a significant difference.
Ultimately, the goal is not just to understand the dangers of e-cigarettes but to take proactive steps toward minimizing their harm. By prioritizing research, education, and policy reform, we can work toward a future where vaping no longer poses a widespread threat to public health. Awareness is the first step—action is what will drive real change.
Image credits Google Labs